#227: Why is Nobody Talking About This?
We are hurtling towards an economic and social disaster for ageing
Hello! I’ve been on the road on a personal emergency, and then trying to catch up desperately before heading off on week and a half of holiday in the Masai Mara and the Serengeti. So apologies for the infrequent updates. Let me leave you with this one - something I’ve been tracking for a while. It’s like we’re on the deck of the Titanic, heading for the iceberg which we can all see, directly in our line of travel, but bizarrely, nobody wants to take the wheel or steer the ship away.
The Future of Care Is the Future of Society
Some problems hide in plain sight but persist because nobody can or wants to solve them, even though everybody can see the problem looming.
A Global Picture
The world population growth peaked in 1968 at 2.1% pa and has been declining since then. It currently stands at 1.1% paAt some point in second half of the 21st century, the world population will start to decline according to most projections.
Additionally, life expectancy has been steadily increasing. Life expectancy is rising across the world – 5 years in the UK, and 10 years for India, 1990-2015. There are moonshot efforts by some businesses to find ways to significantly increase the human lifespan. Many people believe that living well into our hundreds is within reach and that the first person who will live till 200 has already been born.
Overall, this points to a steady increase in the average age of people across the world, and also, a significant rise in the number of people over 65 across the world. As per current trends, by 2050, there will be more than 2 billion people over the age of 60 in the world between 21- 25% of the world’s population. There are already close to 90m people across the top 16 European countries who are 65 years of age.
The UK Snapshot
In the UK, 18% of people (about 11.9m) are 65+ currently. This number is set to reach 25%+ over the next 15 years. The corresponding number for Germany is 17% currently. One of the underlying factors is the rise in life expectancy.
The Challenge
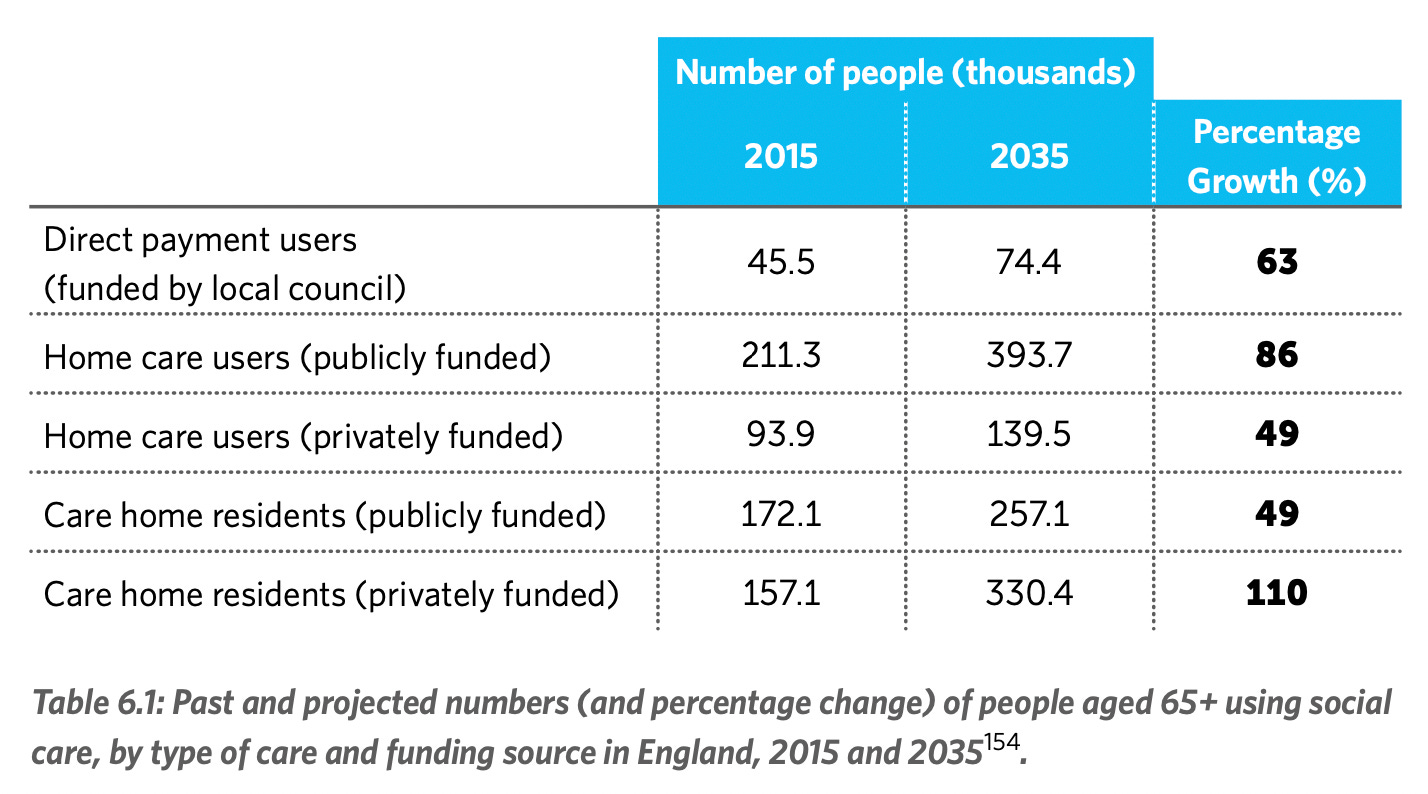
This picture of ageing represents a dual challenge. There is a social care challenge - we don’t have the means, resources, and sometimes even the skills to look after this ageing population at the scale required. This has a significant financial aspect - the combination of pensions and government funding is inadequate to support the needs of older people. The funds may be inadequate to ensure even a very basic quality of life for the 65+. Social and healthcare will form the majority of this cost.
The cost of care home stay in the UK ranges between £30K-50K/yr. The care home sector is in financial distress with costs going up, revenues flat, and subsidies declining, with labour shortages. 81% of councils in the UK have seen a drop in the number of care homes. Scotland has seen a 21% decline in care home capacity 2007-2017. The total public spending on adult social care in 2018/19 was £22.2 bn and an estimated additional £12bn/ year is needed for 2023/24, and approximately 40% of this is for 65+ citizens.
A wide range of problems are linked with ageing:
For example, frailty is associated with an increased risk of falls. Over half of frail adults are reported to have fallen in any given year. In 2017 to 2018 there were around 220,160 emergency hospital admissions related to falls among patients aged 65 and over, with around 146,665 (66.6%) of these patients aged 80 and over. Total Annual Costs to the NHS of falls is £4.4bn, of which £1.1bn goes to social care following surgery.
Let’s remind ourselves how Social Care works today:
It is outside the purview of healthcare historically, so the NHS doesn’t address this problem. Although integrated care boards have been set up recently.
Local government picks up a part of this – especially people who need the support and cannot afford this.
Family members are a big part of the care network and ecosystem
Voluntary organisations make up a significant part of care provision
However, it is common for one person to be ‘looked after’ by multiple people from different organisations who all do specific tasks (e.g. read out letters, handle correspondence, help to walk to the shop, cook, etc.) but don’t share information with each other.
Care Homes are at the institutional end of the spectrum. There are 17,000 care homes in the UK in 2024
There is a shortage of manpower across the organised and unorganised sectors of care, in the UK
Pensions Inadequacy Adds To the Problem
A comfortable living cost in the UK is £54K for a couple. A moderate = £34K, and a basic lifestyle is around £26K. At current levels of pensions, people will just about be able to manage a basic lifestyle.
The bottom line is that pension contributions too low. In the UK, we have largely defined benefits pensions, for which the volume and amount are both low.
The average contribution is on avg 8%, but needed to be 15% (even 20 years ago with higher rates of return).
3 Things Contribute to the pension situation worsening:
Higher rates of self employment rates means lower engagement with Pensions, and lower compulsory savings.
From an environment where more people had defined benefit pensions, we’ve now moved to more people having defined contribution pensions. In a defined contributions scenario, the risk is on the individual who is unprepared for eventualities created by market and interest rate movements.
A drop in owner occupier segment, to more private renting also leads to a longer term challenge as people don’t have an asset to fall back on and there is an increase in inequality.
For the economy, there is a £100 bn annual cost of sustaining pensions with triple lock, even with rise of pension age in the next 50 years; £45 bn by 2050
The Role of Technology
There is therefore a need for us to use technology to bring down the cost of care, and using financial incentives to help people make better choices about health long before they hit the 65 year mark. This has a double benefit as prevention has a substantially higher ROI than curative medine.
Technology can be AI, Sensors, Robots, but its important that tech is not used simply to run things a little better than they currently are, but to actually transform care. AI can help predict care needs, and significantly tune down the knock on effects on the healthcare system. It can dramatically reduce the pressure of resources and optimise across complex needs and providers. Robots can perform tasks and provide emotional support too. Data backbones, and rethinking the delivery of care via the ecosystem is within our grasp.
The problem is that nobody’s really buying this transformation. Individual councils and boards are starting to think about social and health care collectively, but its a bit like trying to fix the climate crisis by buying solutions piecemeal in individual local governments. And it’s also a problem because if left unchecked consumers will end up signing a Faustian bargain with a global tech major of some description.
The time to move is now. We simply don’t know how just yet.
See you soon.





Thank you for this perceptive overview. One of the things that must be taken into account is that 65 is the new 45. In other words, there’s a focus on the frailty of getting older but not the possibilities. Most of the issues you raise are really about the over 75s and maybe even over 80s.
IMV alongside this care and pensions issue is the broader health issue that means we need to shift mindsets to say everyone will be in the worksite much longer (not 2 years but 10 at least) and so needs to be physically and mentally ready for that.
In the UK we have a huge proportion of the workforce at all ages who are unproductive and claiming disability. Technology can play a role in changing that too. This mindset shift is a fundamental issue that can help solve a number of these issues.